Osteoarthritis

What is Osteoarthritis?
Osteoarthritis (OA) is a degenerative joint disease that primarily affects the cartilage, the slippery tissue that covers the ends of bones in a joint. It is the most common form of arthritis and typically develops gradually over time, although it can also occur due to injury or excessive wear and tear on the joints
Patients with osteoarthritis often present with the following symptoms
- Joint pain: Persistent pain, typically worsened by activity and relieved by rest, is a hallmark symptom of OA. The pain may be described as aching, sharp, or dull and is usually located in the affected joint(s).
- Stiffness: Joint stiffness, especially in the morning or after periods of inactivity, is common in OA. It can improve with gentle movement but may worsen with prolonged rest.
- Reduced range of motion: OA can lead to decreased flexibility and difficulty moving the affected joint(s) through their full range of motion.
- Swelling: Inflammation of the joint may result in swelling, tenderness, and warmth around the affected area.
- Crepitus: Patients may experience a grating sensation or sound (crepitus) when moving the affected joint(s) due to the roughening of the cartilage surfaces.

Diagnostic Tests
To diagnose osteoarthritis and rule out other possible causes of joint pain, a physiotherapist may employ various tests and assessments, including:
- Physical Examination: Assessing joint range of motion, strength, stability, and function can provide valuable information about the extent and impact of OA.
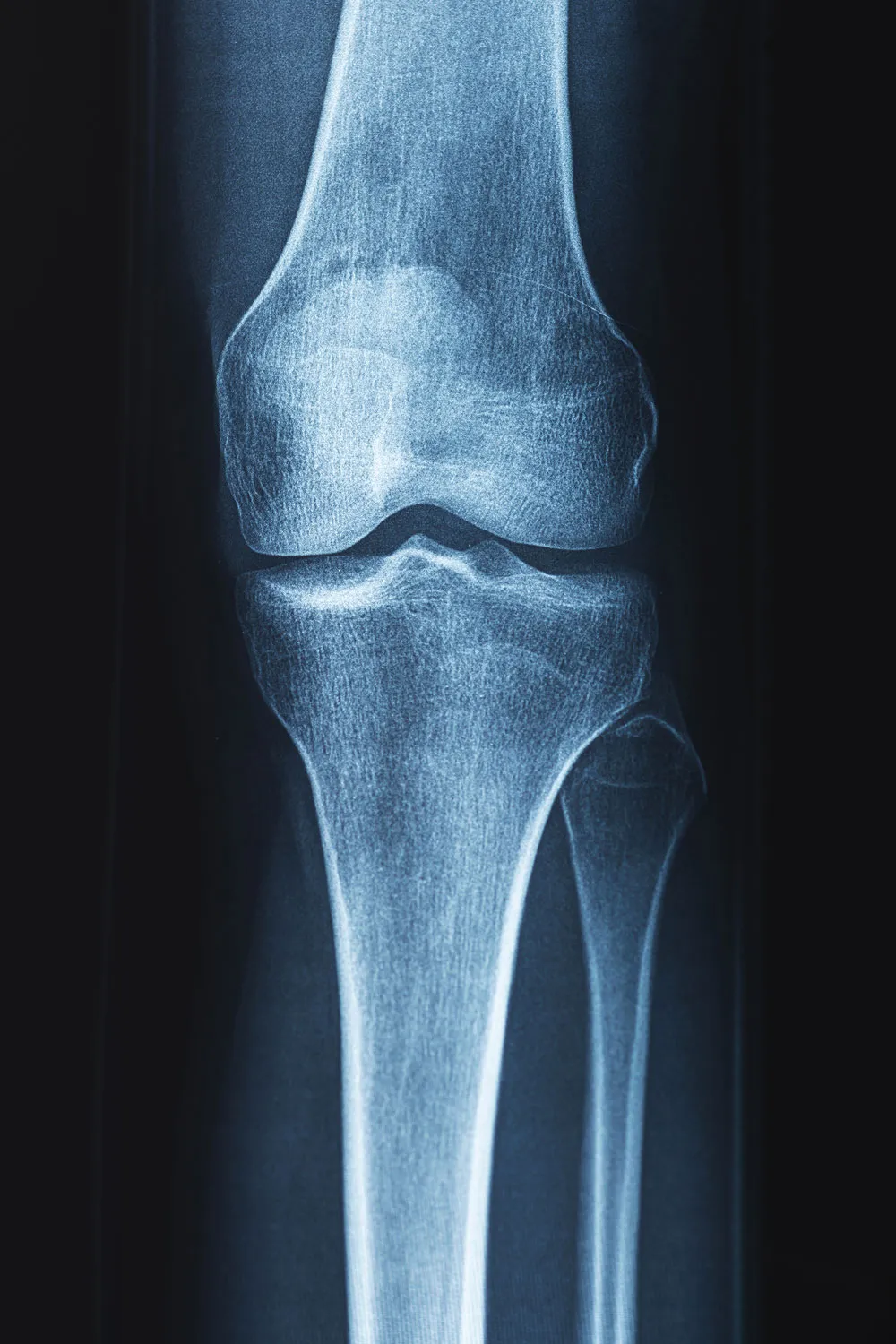
- Imaging Studies: X-rays are commonly used to visualise joint damage, such as narrowing of joint space, bone spurs (osteophytes), and changes in bone density characteristic of OA. MRI scans may also be ordered to assess soft tissue structures, such as cartilage and ligaments.
- Blood tests: Although there is no specific blood test for osteoarthritis, certain blood markers may be elevated in inflammatory forms of arthritis, helping to differentiate between different types of arthritis.
Treatment Methods
Treatment for osteoarthritis aims to relieve pain, improve joint function, and enhance quality of life. From a physiotherapist’s perspective, management strategies may include:
- Exercise: Designing a tailored exercise programme to improve joint mobility, strengthen muscles around the affected joint(s), and promote overall physical fitness can help manage OA symptoms. This may include activities such as swimming, cycling, and gentle stretching exercises.
- Manual therapy: Techniques such as joint mobilisations, soft tissue massage, and manipulation may be used to reduce pain, improve joint function, and enhance mobility.
- Education: Providing patients with information about their condition, including lifestyle modifications, joint protection techniques, and strategies to manage pain and inflammation, can empower them to take an active role in managing their OA.
- Assistive devices: Recommending the use of supportive devices such as braces, orthotics, or walking aids can help reduce stress on affected joints and improve mobility.
- Pain management: In some cases, pain relief medications such as paracetamol or nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to alleviate pain and inflammation associated with OA.





